Information vs. Implementation
How can we respond better to pandemics? Centralize the spread of information—and decentralize policy implementation
By Tina Marsh Dalton
At first, it was a puzzle to researchers. Cell phone data that tracked mobility early in the COVID-19 pandemic just didn’t make sense: Why did individuals’ travel away from home drop steeply as early as March 9, when state stay-at-home orders didn’t start until 10 days later? The answer was simply the power of information.
Evidence suggests that approximately 45% of the increase in social distancing occurred because of information people received—such as first-case announcements and emergency declarations—not because of mandatory policies. More recently, we’ve seen similar information interest regarding mpox, formerly known as “monkeypox.” Google trends data shows that in the U.S., searches for “monkeypox” surged on May 22 of this year, the same week the U.S. announced its first case, and on July 24, one day after the World Health Organization (WHO) declared monkeypox a global health emergency.
Despite a promising start—people attentive and engaged in an emerging public health issue—COVID responses eventually moved to political turmoil over state policy, schools mired in layers of restrictions that were always in flux, and widespread vaccine hesitation. Mpox’s start was not much better. Is this sort of turmoil inevitable?
In a word, no: We can do better to make public health responses faster and more effective. To make crisis response faster, we need timely, clear and widely communicated information. And to make responses more effective, we need to better direct our limited resources with less waste. This can happen if government and local forces each tightly focus on their strengths. The key to both goals is to separate information from implementation.
Learning from Past Mistakes
Centralized government agencies, such as the U.S. Centers for Disease Control (CDC) and the WHO, have been major information providers for both COVID and monkeypox. This role is commonly handed to central government agencies for several good reasons. First, collecting and disseminating information is expensive and requires pre-established networks to connect information to media, local public health agencies and the public. Since these networks are already established, it is cost-efficient for the CDC to reuse them for each health emergency—much like reusing municipal water pipes rather than each utility company installing its own. The same goes for analysis of infection trends. Centralized computing infrastructure and data analysis mean local public health offices don’t have to reinvent the (analysis) wheel.
Second, public health information isn’t like a typical product you might purchase in the grocery store or search for on Amazon. Unlike the latest electronic gadget, information isn’t limited to those who can snap it up on its release date: It can be simultaneously consumed by great swaths of people. Disseminating up-to-date public information from a central source saves time in a crisis. For example, when the genetic code for the novel coronavirus was made available in early January 2020, it was published on an open-access online database that was shared with the world. Researchers in all corners of the globe could get straight to work, without waiting for their local authorities to pass along vital information.
Two promised reforms from the recent CDC internal review can improve the agency’s ability to perform this role. First, the CDC has pledged to restructure its communications office and revamp its websites to make public health guidance clearer and easier to find. This will improve its “pipeline” to get information to more people quickly. Second, the CDC is revamping the kind of employee activity it rewards to move away from focusing on academic publications. While academic articles certainly generate information, this is not an efficient use of the agency’s strengths as a central information provider.
Plentiful private sector organizations are already engaged in academic research, such as universities, hospitals and major medical laboratories. The CDC’s biggest impact is in synthesizing and communicating that information publicly—to improve the quality and frequency of communication in the pipelines it maintains. Moving forward on mpox, CDC efforts should be squarely directed toward getting information to specific at-risk communities.
The problem comes when the provision of information gets mixed with implementation—and the COVID-19 pandemic generated several examples of this. Initial CDC guidance tried to wade into implementation to address mask and personal protective equipment shortages by discouraging the use of masks by the general public. However, this backfired once mask supply recovered and people resisted the CDC’s new mask guidance.
Varying local conditions also complicated centralized implementation. Social distancing guidelines were fixed and quite specific—precisely 6 feet of personal space—but applied widely across a diverse range of settings, from New York City, with high population density and crowded public transportation, to rural Montana, with miles between people and nearly exclusive use of personal vehicles. The same implementation mistakes were made with the January 2022 federal rollout of four free at-home COVID tests. Four tests were authorized, for example, to a Brooklyn multigenerational residence and four to a bachelor’s address in rural Idaho. These policies created waste by misapplying scarce resources at the height of the biggest COVID wave yet.
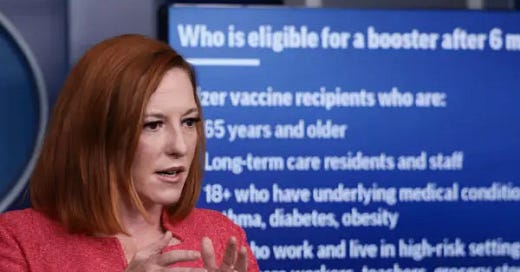
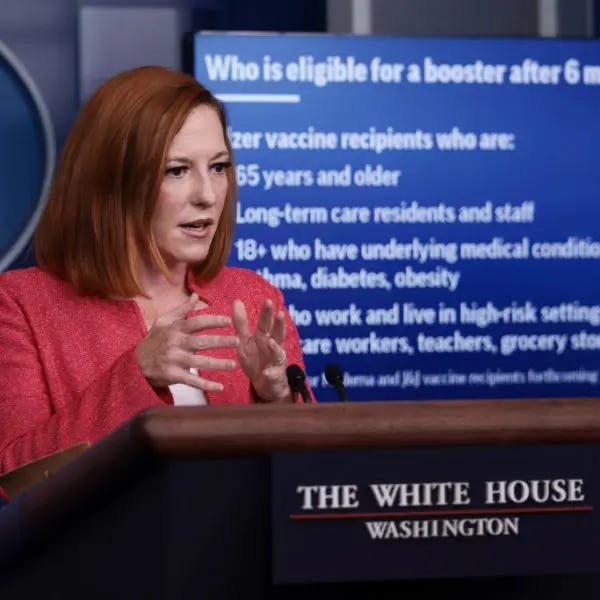
At the other extreme, explicitly attempting to respond centrally to varied local conditions can also generate waste. Vaccine rollout recommendations were often slowed down by minute deliberations about order of access, rather than the simplicity of maximizing shots administered as quickly as possible. For example, West Virginia’s early surprising lead in the delivery of COVID vaccinations was simply because it focused on getting as many shots into arms as possible and using existing provider networks and the National Guard.
In contrast, more than 20 states further subdivided the Advisory Committee on Immunization Practices’ COVID vaccine delivery guidelines for Phase 1a, which were already specific to healthcare workers—creating categories such as “very high,” “high” and “medium” risk categories (as Alabama did) or specific rankings in each group (as Idaho did). Implementation missteps also chipped away at the public’s trust that policymakers understood the realities of the pandemic. A Harvard study found that public opinion of the U.S. public health system dropped from 43% positive down to 34% positive from 2009 to 2021, even while positive ratings of the medical system increased during this period.
Keep Implementation Local
Moving implementation to local forces is more effective. The nature of public health policy is that it requires judgement calls when our best current information bumps up against reality. Local conditions vary by population size, race and ethnicity makeup, age distribution, education and income levels, political unity... shall we stop there in the interest of time? Yet despite varying local needs, all school systems were asked to put into place improved ventilation, 6 feet of social distancing and masking.
However, in the face of these government demands, they often had to deal with insufficient budgets or not enough political will to do all three things. In reality, school authorities had to struggle through tradeoffs: If there wasn’t enough funding for improved ventilation, they prioritized distancing and masks. If distancing wasn’t physically possible, they had to come up with alternative attendance solutions. By contrast, decentralized implementation can empower districts to tailor their actions to the unique concerns and needs of their own messy environment.
Furthermore, decentralizing crisis responses can lead to innovation that not only satisfies guidelines, but creates greater value. Once the value of social distancing was understood, the creativity of entrepreneurs and the power of the internet combined to replace many interactions that previously needed to occur in person—a supremely more effective solution than standing 6 feet apart! Numerous online platforms, such as the ubiquitous Zoom, emerged to offer a way to continue daily businesses operations and social gatherings while eliminating infection risk. By mid-April 2020, Zoom Video Communications had 300 million daily meeting participants worldwide—nearly equal to the size of the entire U.S. population.
Decentralized innovations were as diverse as communities themselves. Streaming concerts and other entertainment—ranging from opera singer Andrea Bocelli to “Metallica Mondays”—emerged for all demographics. Restaurant owners responded with outdoor seating, online ordering and partnering with delivery services such as GrubHub and DoorDash. On the supply side, companies such as Shopify moved businesses to e-commerce, and automation grew in inventory systems. Flexible market solutions kept businesses open, yet customers could take advantage of protective options adapted to their own risk levels—from completely online ordering and delivery, to curbside pickup, to enjoying your meal on the patio.
In recent months, there have been improvements in embracing decentralized responses to the mpox pandemic. Low vaccine and testing availability has left at-risk communities scrambling for vaccines and testing kits. From New York City to Denver to San Francisco, “first doses first”—prioritizing first doses—is being used to make the best of imperfect conditions. This approach prioritizes getting at-risk patients their first dose of a multiple-dose regimen while waiting for more supply to arrive.
This contrasts with the centrally imposed COVID approach, which set aside two doses per individual—meaning that a smaller number of people could receive at least one dose of the multi-dose Pfizer and Moderna vaccines in a short period because available doses were being held for future use. “First doses first” better recognizes the initial hurdle of limiting the spread of infection when faced with the tough reality of scarce doses on hand.
New Successes for an Old Tool
Additionally, there is a new tool just starting to be wielded against mpox that highlights the cost efficiencies and speed of centralized information, but also the flexible effectiveness of local implementation. Sewage testing, which emerged as a novel COVID tool, consists of sampling wastewater for evidence of viral spread. It has been used to track polio infections since the 1940s, which often go undetected because of non-specific symptoms, and was accordingly valuable for the asymptomatic spread of COVID-19.
Sewage testing leverages centralization by essentially testing tens of thousands of individuals with a small team who can quickly transmit results to a central agency and the public. Costs are low compared to individual testing, and it slashes coordination costs between testing agencies and the CDC. It also highlights how the CDC can be an important information aggregator and disseminator without creating the data itself.
Sewage testing is often performed by university collectives or hospitals. The collected information can be analyzed by the CDC’s National Wastewater Surveillance System with its experience in data analysis and synthesizing trends. This repeated experience is important since sewage testing results are not always straightforward—the types of institutions in the catchment area may vary (residential vs. institutional settings); lead time to rising infections is sometimes guesswork; and recent heavy rainfall can dilute samples.
We’ve witnessed a variety of smart approaches to local implementation using sewage testing information. As recently as August 2022, New York City mounted a vaccination campaign in areas where sewage testing showed an uptick in polio infection. Australia and New Zealand heavily relied on sewage testing to take early action on COVID outbreaks in previously low infection areas. This is similar to California’s current use with mpox, to better direct scarce testing resources. Municipalities have also used sewage testing to inform the back end, to confirm that cases were waning after the omicron wave. Sewage testing provided a double-check that allowed strained public health resources to move on to more pressing needs.
The CDC and other governmental health agencies lost substantial public trust during the COVID-19 pandemic. As we grapple with the growing mpox epidemic and the ebb and flow of new COVID strains, we can use the past to improve future responses. Timely, direct information has consistently led to protective individual responses and better targeted public health campaigns. We can mount stronger responses by commissioning central government agencies to focus primarily on providing updated information and national-level analysis. Armed with this information, the details of implementation should be moved into the hands of local public health agencies and businesses to create flexible solutions that adjust for local limitations, or, better yet, innovate the crisis away.